Perioperative Frailty Assessment and Mitigation - #117
Take QuizEvaluate and manage frailty in the perioperative setting.
Frailty is a distinct clinical syndrome characterized by multisystem physiological decline with increased vulnerability to stressors and adverse clinical outcomes (i.e., reduction in physiological reserve). This is especially evident in the perioperative period, where frailty is strongly associated with an increased 30-day mortality risk and complications (RR 3.71 & 2.39, respectively)4,5. Older adults with frailty are also at Increased risk for adverse perioperative events including post-operative delirium, prolonged length of stay, and discharge to a higher level of care (e.g., assisted living facility, nursing home). Frailty is associated with poor perioperative outcomes, and frailty assessment using a validated tool is recommended in clinical practice guidelines. Validated tools recommended to screen for frailty in the perioperative setting include:
- “Frail Scale”– this screening tool measures physical frailty and takes approximately 3 minutes to complete. It relies on patient self-reporting, with scores ≥ 3 being consistent with a frail state.
- “Risk Analysis Index” (RAI) - this screening tool is validated in the perioperative setting and takes approximately 3 minutes to complete. It relies on patient self-reporting or caregiver-reporting and is supplemented by the provider’s best clinical judgment. Scores ≥ 37 are consistent with a frail state.
- “Mini Nutritional Assessment” -- this short, validated tool, calculates a score to determine if someone is at risk of malnutrition or is malnourished.
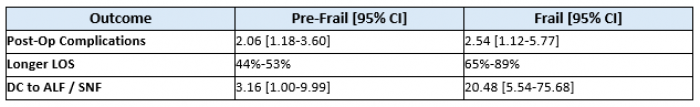
Older adults who screen positive for pre-frail and frail states encounter worse outcomes than their non-frail counterparts.
Once frailty is identified, mitigation strategies should be implemented and may include:
- High protein diet and targeted physical activity
- Anticipatory guidance provided to patients, families, and surgical team to help mitigate risk and understand possible patient trajectories
- Social work involvement for post-hospital disposition planning
- Implementation of recovery protocols such as Enhanced Recovery After Surgery (ERAS) if in-line with hospital protocols (10)
Older adults in the perioperative setting.
Screen patients > 65 years old for frailty in the perioperative setting. When identified, frail patients should be advised that their risk for adverse outcomes is higher than reflected in commonly used perioperative risk calculators. Mitigation steps should be implemented, as time allows, to optimize patients.
More than 50% of surgeries are performed in adults > 65 years of age in the US (7). Frailty is associated with a higher risk of increased length of hospitalization, increased risk of discharge to a higher level of care post operatively, and a higher risk of post-operative complications.
1. Understand the impact of frailty on perioperative risk
2. Utilize tools to identify patients with frailty (or at risk for frailty)
3. Implement steps to mitigate risk for adverse outcomes
- Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–M156.
- Mini nutritional assessment - ® Société des Produits Nestlé SA, Trademark Owners. © Société des Produits Nestlé SA 1994, Revision 2009.
- Hall DE, Arya S, Schmid KK, Blaser C, Carlson MA, Bailey TL, Purviance G, Bockman T, Lynch TG, Johanning J. Development and Initial Validation of the Risk Analysis Index for Measuring Frailty in Surgical Populations. JAMA Surg. 2017 Feb 1;152(2):175-182. doi: 10.1001/jamasurg.2016.4202. PMID: 27893030; PMCID: PMC7140150.
- Tjeertes EKM, van Fessem JMK, Mattace-Raso FUS, Hoofwijk AGM, Stolker RJ, Hoeks SE. Influence of Frailty on Outcome in Older Patients Undergoing Non-Cardiac Surgery - A Systematic Review and Meta-Analysis. Aging Dis. 2020 Oct 1;11(5):1276-1290. doi: 10.14336/AD.2019.1024. PMID: 33014537; PMCID: PMC7505262.
- McIsaac DI, Aucoin SD, Bryson GL, Hamilton GM, Lalu MM. Complications as a Mediator of the Perioperative Frailty-Mortality Association. Anesthesiology. 2021 Apr 1;134(4):577-587. PMID: 33529334.
- Dall TM, Gallo PD, Chakrabarti R, West T, Semilla AP, Storm MV. An aging population and growing disease burden will require a large and specialized health care workforce by 2025. Health Aff (Millwood). 2013 Nov;32(11):2013-20. doi: 10.1377/hlthaff.2013.0714. PMID: 24191094.
- Kwok, V.KY., Reid, N., Hubbard, R.E. et al. Multicomponent perioperative interventions to improve outcomes for frail patients: a systematic review. BMC Geriatr 24, 376 (2024). https://doi.org/10.1186/s12877-024-04985-4
- Mohanty S, Rosenthal RA, Russell MM, Neuman MD, Ko CY, Esnaola NF. Optimal Perioperative Management of the Geriatric Patient: A Best Practices Guideline from the American College of Surgeons NSQIP and the American Geriatrics Society. J Am Coll Surg. 2016 May;222(5):930-47. doi: 10.1016/j.jamcollsurg.2015.12.026. Epub 2016 Jan 4. PMID: 27049783.